Rabia Malik, MD, Asst. Professor, Rush University Medical Center
Recap: Conquer MG Webinar – August 30, 2020
In mid-March 2020, the U.S. Congress approved emergency use of telehealth services in response to the COVID-19 pandemic. This allows patients to receive medical care from their homes through the use of smartphones, tablets or computers.
Rabia Malik, MD, recently explained to the Conquer MG audience how they can make the most of telemedicine visits with their doctors. Dr. Malik practices at Rush University Medical Center. She is an Assistant Professor, Department of Neurological Sciences; Director, MDA Care Center; and Director, RUMC EMG Lab.
Click to watch the video presentation.
Click here to print a summary of guidance for your telemedicine visit.
Preparing for your video visit
 For your visit, you will need:
For your visit, you will need:
- Smart phone or ipad. It should be fully charged. If it’s not charged, make sure it’s connected to a power source. Alternatively, you can use a laptop or desktop computer with camera. However, some apps are not supported on the laptop or desktop, and so the experience may be easier and more efficient on your phone. Be sure to prepare your device in advance.
- Internet connection
- Instructions from your healthcare provider’s office
- Download the app. Your doctor’s office staff will tell you how to download the app onto your device, and how to access your visit. The app is usually free.
Set up needs to happen a few days before your clinic visit, especially if it’s your first time using the app.
- Sign into your patient portal or app to ensure that you have the correct login information and password. If you have problems getting into the application, now’s the time to troubleshoot.
- Appointments can be accessed through a link sent via text to your phone or email. You just need to click the link.
- If you’re using an app, each one is a little different. Usually there is a section in the app that lists your upcoming e-visits. You can go into that section and see details about the visits you have scheduled. When it’s time for your visit, click into it and connect.
- The clinic staff should be able to help you trouble shoot. If you have questions, call the office and have them work through the app with you.
- It often helps to have a family member provide tech support and hold the camera/device.
On the day of the visit…
- Log in 15 minutes prior to your visit.
- Position yourself in a quiet and private area.
- Minimize noise, distractions (turn off TV).
- Make sure the room is well-lit.
- Avoid eating and drinking, just as you would in a clinic visit.
- Be patient as you may encounter technical challenges like video freezing, audio lag (It’s also challenging for your doctor!)
Your visit will start like an in-clinic visit.
- Your neurologist will confirm identifying information such as your name and date of birth.
- If it’s your first visit be prepared to talk about:
- A timeline of your symptoms (when did it start, how did it progress?)
- Medical history (your other risk factors, for instance, stroke, high blood pressure)
- Family history (we’re looking for certain risk factors, such as another family member who has an autoimmune disease)
- Social history (where you work, if you live by yourself, history of smoking and alcohol consumption)
- Current medications (keep a list of all meds you take so we can make sure our records are up to date)
- Allergies (we want to know if you’re allergic to any medications)
Virtual Neurological Exam
This part of the exam is different from an in-person visit. You can take several steps to ensure we get the information needed.

Image of woman centered, facing straight forward, with light source illuminating face and background

Image of woman sitting centered with light source behind her creating dark shadow
Light source and camera position. We will want to be able to see your face clearly. Position yourself to face a light source. A large part of the exam is the strength of your eyes and face, so it needs to be illuminated. The light should not be behind you.

Woman sitting centered, forward facing, in total view
Position your camera so the whole face can be seen. We need to check your face for symmetry, for instance, to see if the eyelid on one side droops more than the other side. A caregiver or family member can positon the camera for you. If you’re by yourself, prop the camera with books or boxes. Get the camera close to your eye level.
The Virtual Exam Components
- Eye and facial movements can be assessed over a video visit. It’s important that you sit where your face is well-lit, and your camera is positioned so we can get a good view of your full face.
- Ptosis fluctuations (drooping eyelids) can be assessed as well, as long as the camera is well-positioned.
- Speech assessment. We will listen for slurred speech and fatigability.
- Be prepared to walk so your gait can be assessed. If you are at risk for falling, make sure a family member is present to provide support. If you are by yourself, one way to be prepared is to prop the camera on a chair, vertically. (In other words, you’ll need a second station where you can prop up your camera.) The lower level of the camera allows us to see the whole body from head to toe. We can assess how you walk (your gait), plus do a component of the strength exam in the legs.
Mobile device propped straight up by books on chair
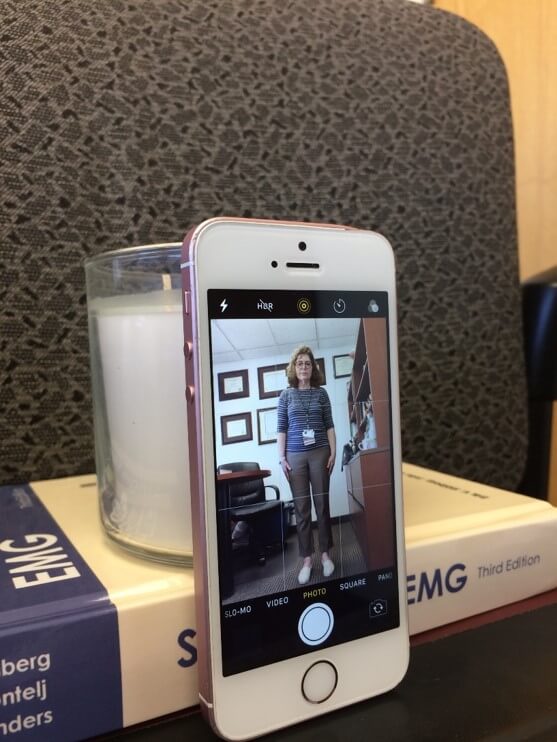
View of full body as seen on mobile device propped up by books on chair
Vital signs
– weight, temperature, and blood pressure – can be recorded if you have access to a scale, thermometer, and/or blood pressure cuff on the day of your exam.



Mental status
will be checked. We’ll ask questions to check your orientation, comprehension, memory and language.
- The strength exam is limited when you do a virtual exam. When you come to the clinic, your muscle strength is tested by “confrontation.” This means you push against your doctors hands, so it’s your effort against our effort. Your doctor assesses where muscle weakness occurs. In a virtual exam that’s not possible. However, we can get a rough estimate of muscle strength.
- We can ask you to raise the arms above your head. First, Can you do it? Second, can you sustain it, or is there fatigability with arm elevation?
- Next we’ll ask you to do slow finger taps, tapping each digit to the thumb one after another. That gives an assessment of how weak the finger muscles are.
- We can assess strength of the hip muscles by seeing if you can stand up from a chair easily, with arms crossed. That tells whether hip muscles are strong.
- Similarly, for trunk muscles we see how easily you can get up from a bed.
- We may have you stand on one leg at a time, or stand on your toes or heels. That gives us a sense of the strength in the leg muscles.
- The sensory exam is limited as well. But with the help of a caregiver or family member, we can determine if there are any differences in sensation between your left and right sides. That person can rub their hands over each of your arms, and you can report if it’s the same sensation or different. You also can demonstrate whether there is a difference between the upper part of the arms and legs (the proximal) and the lower part (or distal). If there is no one available, we may ask you to draw an imaginary line around the area of numbness.
Typically, sensory symptoms problems are not part of MG. So the more important parts of the exam are the face, strength exam of arms and legs, and speech changes during the interview.
End of your visit
At the end of the visit, be sure to:
- Ask your questions. Keep your list ready.
- Summarize the recommendations and plan with your neurologist. For example if you’ve been given a change in medications, make sure you know the amount and schedule change.
Your doctor can e-prescribe your meds, and place orders for lab, bloodwork and imaging studies. Although you may be hesitant to come to the hospital for blood draws and studies, keep in mind there are regulations and precautions in place to prevent you from being exposed to many people in a room. For instance, many places require that you come by appointment to get blood tests. This ensures fewer people are in the waiting room.
When is an in-person visit needed?
It’s important for a doctor to see you in person when:
- You have significant changes in your MG
- A change in medications is made
- Detailed examination is needed
- New patient visit
- Red flags: swallowing difficulties, feeling short of breath with little activity and neck weakness
Keep in mind, clinics and hospitals are taking special precautions against COVID-19.
- Mask are required
- Patients are social distanced in waiting rooms
- Surfaces are wiped down regularly with disinfectants
- With each patient, the office will review symptoms of COVID-19
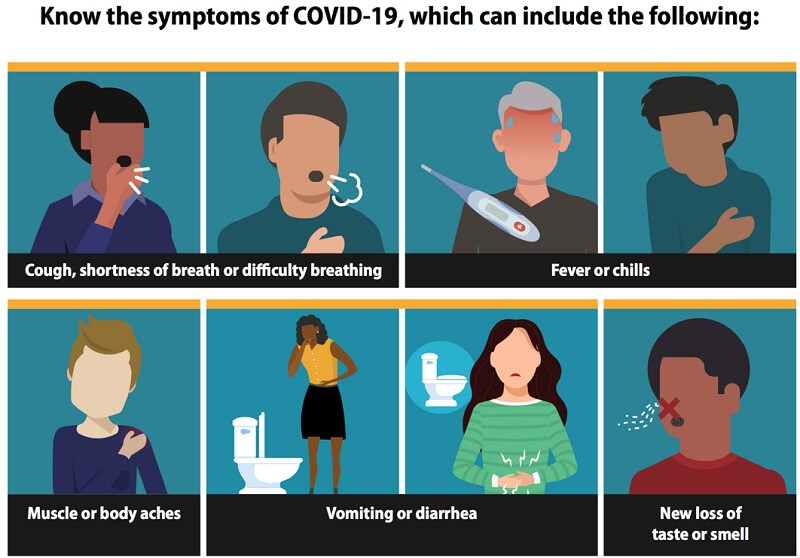
Vector graphic image of covid-19 symptoms